Modern distribution systems are as efficient in spreading viruses as they are moving goods. But, as we weather the increasingly pessimistic media coverage, we can at least put past learnings to use.
I’m not a health expert – but I do have first-hand experience of this.
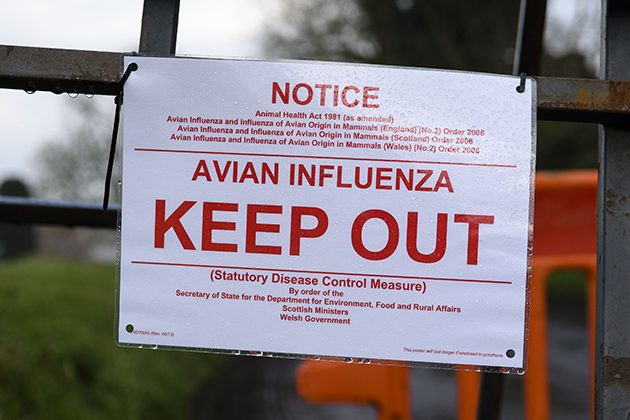
Seeing the current coronavirus emergency takes me back 15 years to the Bird Flu epidemic. At the time I was the distribution manager for a company that produced and supplied frozen food for the care sector through a network of facilities served by an overnight trucking operation.
The outbreak of Bird Flu presented a dilemma. On the one hand we were interfacing with high risk and vulnerable groups across the country, with an unbroken chain of face-to-face personal contact. On the other, we offered a critical specialist service to a healthcare sector which was potentially going to be under serious pressure - so closing down was not an option.
Therefore, we put in place contingency measures to reduce the risk of our distribution network spreading the virus with the support of what is now NHS England. These measures focused on three key principles: minimising face-to-face contact between staff, and between staff and customers, segregating teams and sharing skills, and adopting sanitising protocols.
Coming back to the present, and the current global outbreak of coronavirus, media coverage in recent days has focused on the economic impact, and in particular staff sick absence. Much of this is hypothetical but it’s still prudent that organisations consider contingency arrangements. So what would I suggest to distribution organisations based on my own experience?
- Reduce the risk by splitting staff into self-contained teams with the skills to cover all core functions.
- Keep teams isolated from each other to prevent infection spreading, and use rotas to have teams working on different days.
- Focus on what is required to run the core operation, and who in the organisation has the skills to cover these roles. Consider people from administrative/corporate functions which, while valued in normal times, are not critical to the core operation. Plan ahead and train them in advance to cover any gaps.
- Minimise face-to-face contact. Review your operation and note each and every face-to-face contact that occurs whatever the reason, e.g. morning driver briefings, drivers and other staff meeting in the canteen, staff meeting customers etc. Then think if and how these scenarios may be avoided. For example, an arrangement where drivers collect keys and delivery notes without coming into the despatch office, or creating other designated staff rest areas.
- Any shared equipment – for example, PCs, desks, phones, and vehicles - is a potential source of contamination. Therefore consider the key touch points in your organisation, and set up a check list and sanitising protocol. Issue each staff member with an alcohol-based hand sanitiser and protective gloves so that they can sanitise everything they touch or use at the beginning and end of the shift; get incoming staff to do the same before they start as, by duplication, you are further reducing risk.
- Whilst technology has reduced the reliance on paperwork (which can potentially absorb a virus), any required paper needs to be placed in sanitised plastic pockets by the user. Always sanitise hands after handling paper.
And, of course, follow the official NHS guidance as a minimum.
It’s hard to avoid getting drawn into the media coverage, but the points I make here are about sensible planning - not panicking. This means reviewing your operation, creating a detailed plan, and then communicating it with all staff and doing the requisite training.
Of course, you may not need it in the end. But if you do, you’re better positioned to ride out the uncertainty that lies ahead.

